Unveiling the Role of Cytoplasm Transfer in IVF: Nurturing Egg Cell Growth
In the realm of assisted reproductive technology, cytoplasm transfer has emerged as a revolutionary technique with the potential to enhance the success of in vitro fertilization (IVF) treatment. This innovative procedure involves the transfer of cytoplasm, the gel-like substance inside a cell, from a healthy donor egg to the recipient egg of a woman undergoing IVF. In this article, we delve into the intricate role of cytoplasm transfer in nurturing egg cell growth and its impact on the outcomes of IVF treatment.
Understanding Cytoplasm Transfer
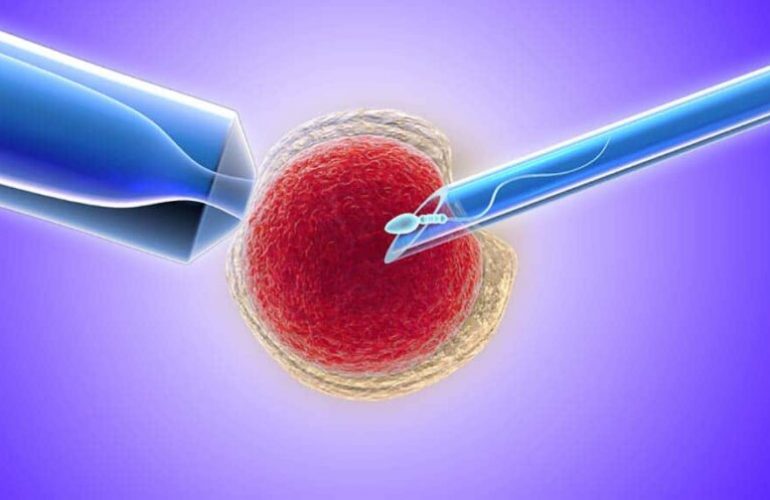
Transfer of cytoplasm is a technique used in IVF to improve the quality of eggs and increase the chances of successful fertilization and embryo development. The cytoplasm contains essential components such as mitochondria, which are responsible for producing energy within the cell. By transferring cytoplasm from a healthy donor egg, the recipient egg gains access to these vital components, potentially enhancing its developmental potential.
How Does Cytoplasm Transfer Affect Egg Cell Growth?
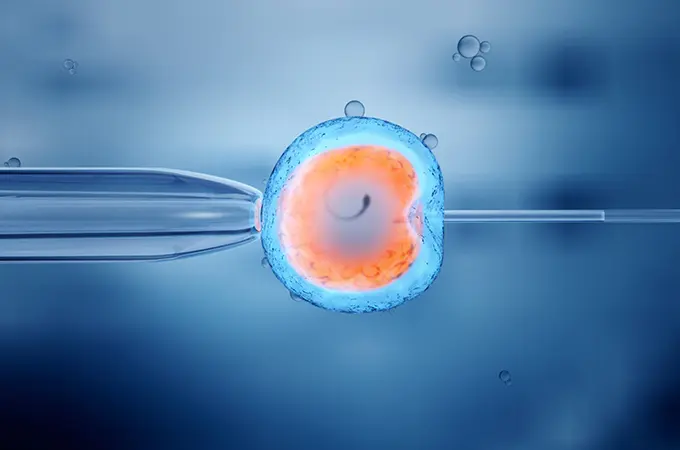
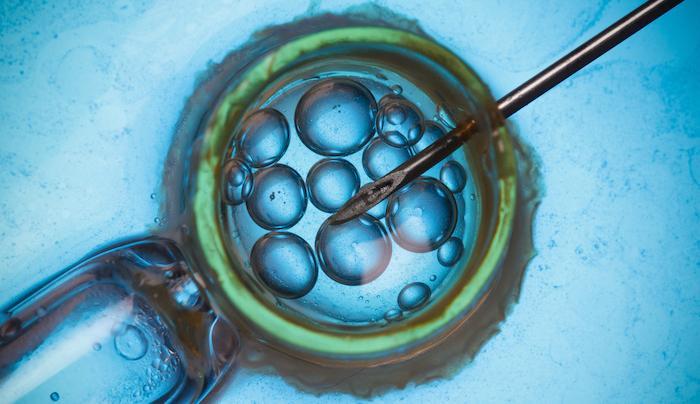
The process of this procedure begins with the extraction of cytoplasm from a healthy donor egg. This cytoplasm is then injected into the recipient egg, supplementing its existing cytoplasmic content. The transferred cytoplasm contains crucial organelles and molecules that can stimulate cell division, improve mitochondrial function, and enhance overall egg cell health.
One of the key ways cytoplasm transfer affects egg cell growth is by rejuvenating the recipient egg. As women age, the quality of their eggs can decline due to factors such as decreased mitochondrial function and increased oxidative stress. Cytoplasm transfer can help mitigate these age-related changes by providing the recipient egg with fresh, healthy cytoplasm, thereby improving its ability to develop into a viable embryo.
The Impact on IVF Treatment
The use of cytoplasm transfer in IVF treatment has shown promising results in improving the outcomes of IVF cycles. Studies have reported higher fertilization rates, improved embryo quality, and increased implantation rates in women who undergo this procedure as part of their IVF treatment.
Furthermore, cytoplasm transfer may be particularly beneficial for women with certain infertility issues, such as poor egg quality or recurrent IVF failure. By enhancing the developmental potential of their eggs, cytoplasm transfer can increase the likelihood of a successful pregnancy for these women.
Factors Influencing the Success of Cytoplasm Transfer in IVF Treatment
Cytoplasm transfer is a promising technique in in vitro fertilization (IVF) treatment, offering potential benefits for women struggling with infertility. However, the success of cytoplasm transfer can be influenced by several factors that need to be considered. In this article, we explore the key factors that can impact the success of cytoplasm transfer in IVF treatment.
Quality of the Donor Cytoplasm
The quality of the donor cytoplasm plays a crucial role in the success of cytoplasm transfer. The cytoplasm contains essential organelles, such as mitochondria, which are responsible for energy production within the cell. High-quality donor cytoplasm with healthy mitochondria can provide the recipient egg with the necessary components for optimal development.
Compatibility Between Donor and Recipient Eggs
The compatibility between the donor and recipient eggs is another important factor in the success of cytoplasm transfer. The donor cytoplasm should be compatible with the recipient egg to ensure that the transferred cytoplasm is accepted and utilized effectively. Factors such as genetic compatibility and the stage of the recipient egg’s development can influence this compatibility.
Technique and Expertise of the IVF Clinic
The technique and expertise of the IVF clinic performing the procedure are critical factors in determining its success. The procedure requires precision and skill to ensure that the cytoplasm is transferred effectively and without damaging the recipient egg. Clinics with experience in cytoplasm transfer and a high success rate in IVF procedures are more likely to achieve positive outcomes.
Health and Age of the Recipient
The health and age of the recipient also play a role in the success of this procedure. Younger women tend to have healthier eggs with better developmental potential, which can improve the success rate of cytoplasm transfer. Women with underlying health conditions or age-related issues may not respond as well to cytoplasm transfer.
Underlying Causes of Infertility
The underlying causes of infertility in the recipient can also impact the success of the transfer process of cytoplasm. Women with certain infertility issues, such as poor egg quality or recurrent IVF failure, may benefit more from this procedure than others. It is essential to address these underlying causes to optimize the chances of success.
Conclusion: Enhancing Egg Cell Growth with Cytoplasm Transfer in IVF
In conclusion, cytoplasm transfer represents a promising advancement in the field of IVF, offering new hope to couples struggling with infertility. By supplementing the recipient egg with healthy cytoplasm, this advanced procedure can improve egg cell growth and enhance the success of IVF treatment. As research in this area continues to evolve, cytoplasm transfer holds the potential to further revolutionize the field of assisted reproduction, offering new possibilities for couples on their journey to parenthood.
For more information about this procedure, and its enhancing properties on an egg cell please refer to this blog post by Cyprus American IVF.
For any of your fertility problems, please do not hesitate to contact us. At Fertility Solutions we pride ourselves with the excellent tailored personal care we provide to our patients for their specific needs. A team member will contact you as soon as we get your message, and construct a personal treatment plan for your fertility problems in the country of Cyprus. You can also contact our clinics directly through the links below.
Cyprus Crown IVF Contact: https://en.cypruscrownivf.com/contact
Cyprus American IVF Contact: https://www.cyprusamericanivf.com/contact-us/
Dr. Halil Ibrahim Tekin (Dr. HIT) Youtube: https://www.youtube.com/@dr.halilibrahimtekin1715
Cyprus American IVF Youtube: https://www.youtube.com/@AmerikanTupBebekMerkezi