Clinics in the UK Offering AMH Testing
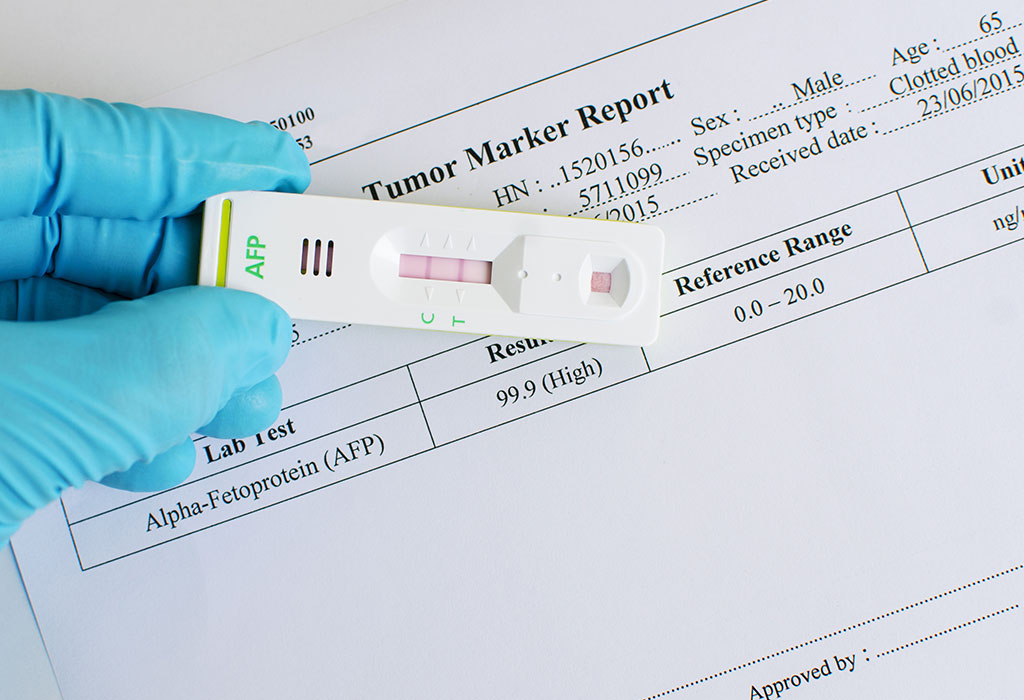
In this article we will explore the best places to get your AMH test in the UK. Anti-Müllerian Hormone (AMH) testing is an essential tool in assessing a woman’s ovarian reserve and overall fertility potential. This blood test helps individuals and couples understand their reproductive health, aiding in decisions about family planning, fertility treatments, or simply gaining insight into their biological clock. Fortunately, numerous clinics across the UK provide AMH testing services, either as standalone tests or as part of broader fertility assessments.
What Is an AMH Test?
The AMH test measures the level of Anti-Müllerian Hormone in the blood, which is produced by small follicles in the ovaries. Higher levels of AMH typically indicate a greater ovarian reserve, while lower levels suggest a diminished reserve. The test is particularly useful for:
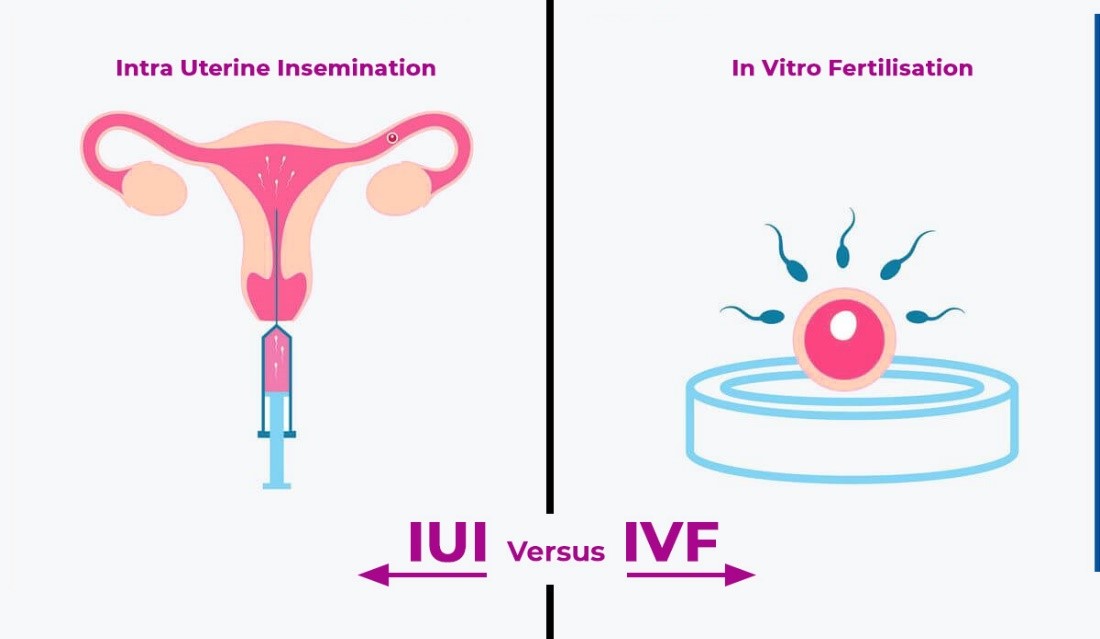
- Women considering fertility treatments like IVF
- Those wanting to assess their fertility status for future family planning
- Diagnosing conditions such as polycystic ovary syndrome (PCOS) or premature ovarian insufficiency
Why Is AMH Testing Required Before IVF or Egg Donation?
AMH testing is a critical prerequisite for fertility treatments, including IVF and egg donation, for several reasons:
- Determining Suitability for IVF with Own Eggs: The test helps fertility specialists evaluate whether a woman has enough ovarian reserve to proceed with IVF using her own eggs. If AMH levels are very low, alternative options such as egg donation may be recommended.
- Customizing IVF Protocols: AMH levels guide the selection of stimulation protocols for IVF, ensuring that medication dosages are tailored to the individual’s ovarian response.
- Predicting IVF Outcomes: Higher AMH levels are often associated with a greater number of eggs retrieved during IVF, increasing the chances of successful fertilization and embryo development.
- Assessing Egg Donation Eligibility: For egg donors, AMH testing ensures that the donor’s ovarian reserve is sufficient to meet donation requirements.
Our clinics require AMH testing as a fundamental part of the fertility assessment to provide the most effective and personalized treatment options for patients.
Clinics in the UK Offering AMH Testing
- London Women’s Clinic
- Locations: Multiple locations, including Harley Street (London), Cardiff, and Bristol.
- Services: Offers AMH testing as part of comprehensive fertility assessments and standalone tests.
- Website: londonwomensclinic.com
- CARE Fertility
- Locations: Clinics nationwide, including Manchester, Birmingham, and Northampton.
- Services: Provides AMH tests as part of fertility evaluations. The results help design personalized treatment plans.
- Website: carefertility.com
- The Agora Clinic
- Location: Brighton, Sussex.
- Services: Specializes in fertility treatments and offers AMH testing for individuals or couples starting their fertility journey.
- Website: agoraclinic.co.uk
- Create Fertility
- Locations: Clinics in London, Manchester, Birmingham, and Bristol.
- Services: Known for their focus on natural and mild IVF. AMH testing is included in their fertility assessments.
- Website: createfertility.co.uk
- Bourn Hall Clinic
- Locations: Cambridge, Colchester, and Norwich.
- Services: Provides AMH tests as part of fertility check-ups and pre-treatment evaluations.
- Website: bournhall.co.uk
- The Fertility Partnership
- Locations: Multiple clinics, including Oxford, Southampton, and Glasgow.
- Services: Offers AMH testing along with other diagnostic tools to provide a clear picture of fertility health.
- Website: thefertilitypartnership.com
- Harley Street Fertility Clinic
- Location: Harley Street, London.
- Services: Provides standalone AMH testing and in-depth fertility consultations.
- Website: hsfc.org.uk
- ABC IVF
- Locations: Clinics in London, Birmingham, and Manchester.
- Services: Offers affordable AMH testing and fertility treatment packages tailored to individual needs.
- Website: abcivf.com
How to Choose the Right Clinic
When selecting a clinic for AMH testing, consider the following factors:
- Proximity: Choose a clinic close to your home or workplace for convenience.
- Cost: Prices for AMH tests can vary, so compare costs across clinics.
- Reputation: Look for clinics with positive reviews and a proven track record in fertility care.
- Additional Services: Some clinics offer bundled packages that include AMH testing along with other fertility assessments, which may be more cost-effective.
- Specialist Expertise: Clinics specializing in fertility care often provide more tailored advice based on your AMH levels.
What to Expect During an AMH Test
The AMH test is a straightforward blood test that can be performed at any time during the menstrual cycle. After the blood sample is taken, results are typically available within a few days. Your healthcare provider will explain the results and discuss any implications for your fertility.
Conclusion
AMH testing is a vital step in understanding fertility health, and numerous clinics across the UK provide this service. Whether you’re exploring fertility treatments or simply seeking insight into your reproductive health, the clinics listed above offer reliable and professional services. Consult with your chosen clinic to determine the best approach for your needs and take the first step toward understanding your fertility.
For any of your fertility problems, please do not hesitate to contact us. At Fertility Solutions we pride ourselves with the excellent tailored personal care we provide to our patients for their specific needs. A team member will contact you as soon as we get your message, and construct a personal treatment plan for your fertility problems in the country of Cyprus. You can also contact our clinics directly through the links below.
Cyprus Crown IVF Contact: https://en.cypruscrownivf.com/contact
Cyprus American IVF Contact: https://www.cyprusamericanivf.com/contact-us/
Dr. Halil Ibrahim Tekin (Dr. HIT) Youtube: https://www.youtube.com/@dr.halilibrahimtekin1715
Cyprus American IVF Youtube: https://www.youtube.com/@AmerikanTupBebekMerkezi