Navigating Fertility Medications in the USA: What You Need to Know
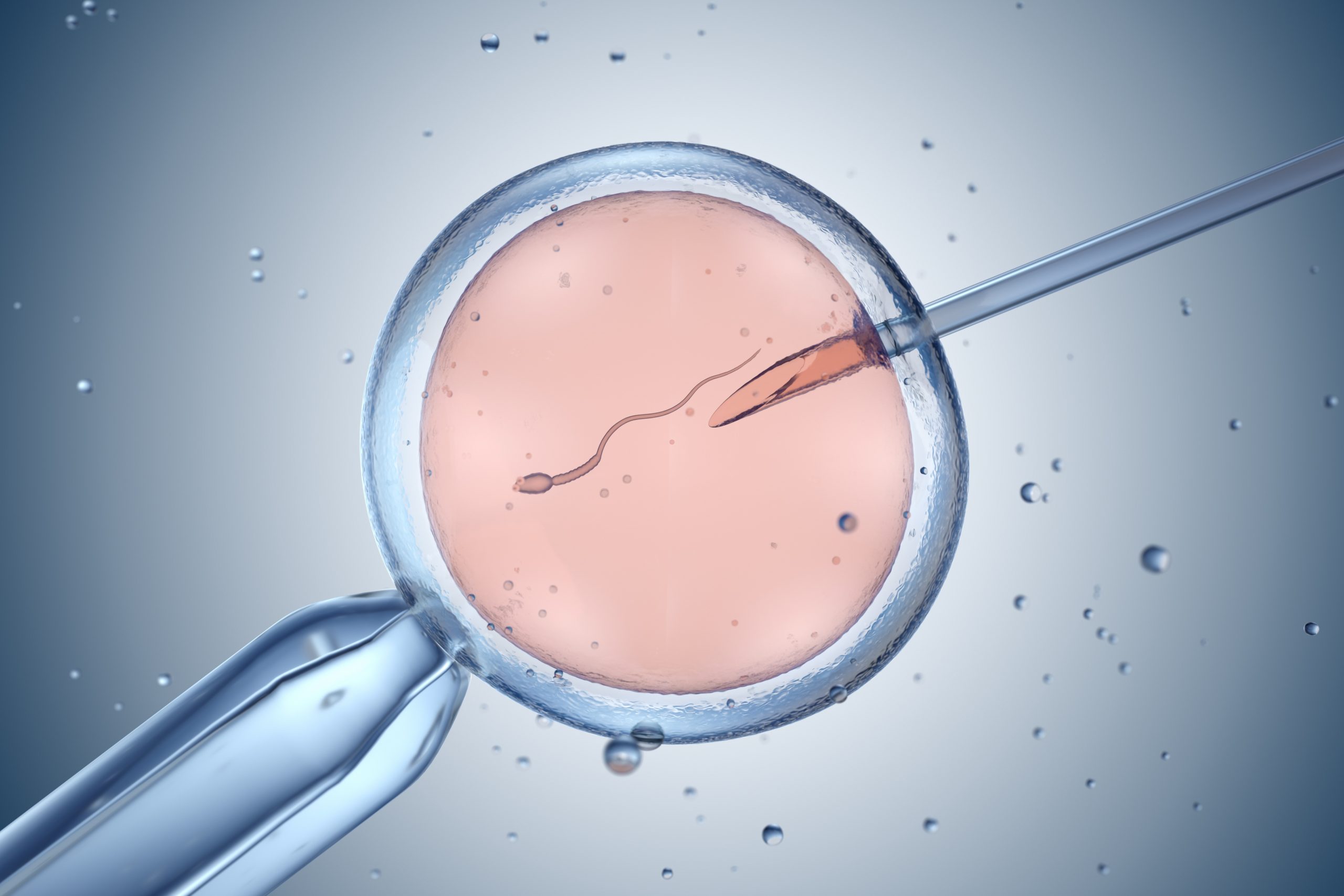
Fertility treatments such as IVF, egg donation, and sperm donation have helped millions of people grow their families. But one of the most crucial parts of any assisted reproductive journey is the use of fertility medications — from stimulating ovulation to preparing the uterus for implantation.
If you’re starting your path to parenthood, understanding how to access fertility medications in the USA is essential. Here’s a step-by-step guide to help you understand where to start, what’s required, and how to safely and legally obtain these medications.
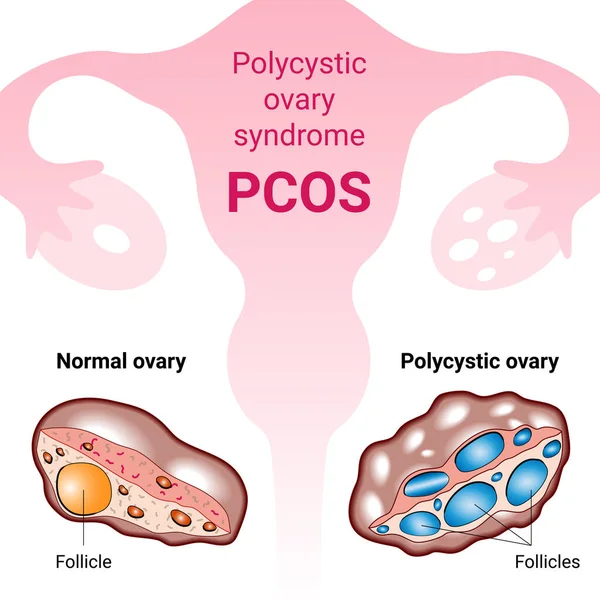
🧬 Why Are Fertility Medications Necessary?
Whether you’re undergoing IVF, IUI, egg donation, or sperm donation, medications are critical to the process. They help:
-
Stimulate the ovaries to produce multiple eggs
-
Regulate or induce ovulation
-
Prepare the uterine lining for implantation
-
Support early pregnancy
These medications are usually prescribed in precise doses and must be taken at specific times in your cycle, often with guidance from a fertility clinic.
👩⚕️ Step 1: Consult a Fertility Specialist
To obtain fertility medications in the USA, you must have a prescription. This begins with a visit to a fertility clinic or reproductive endocrinologist. They will:
-
Review your medical history
-
Conduct tests (bloodwork, ultrasound, semen analysis)
-
Design a customized treatment plan
-
Prescribe the necessary medications based on your protocol
You cannot legally or safely purchase these medications without a prescription.
💉 Common Fertility Medications in the USA
Here are examples of medications often used in various treatments:
For IVF:
-
Gonal-F, Follistim, Menopur: stimulate multiple egg production
-
Ovidrel or hCG trigger shot: triggers final maturation before egg retrieval
-
Progesterone (injections, suppositories): supports the uterine lining after embryo transfer
For Egg Donation (Recipient):
-
Estrogen (pills, patches): to thicken the uterine lining
-
Progesterone: to maintain a receptive environment for the embryo
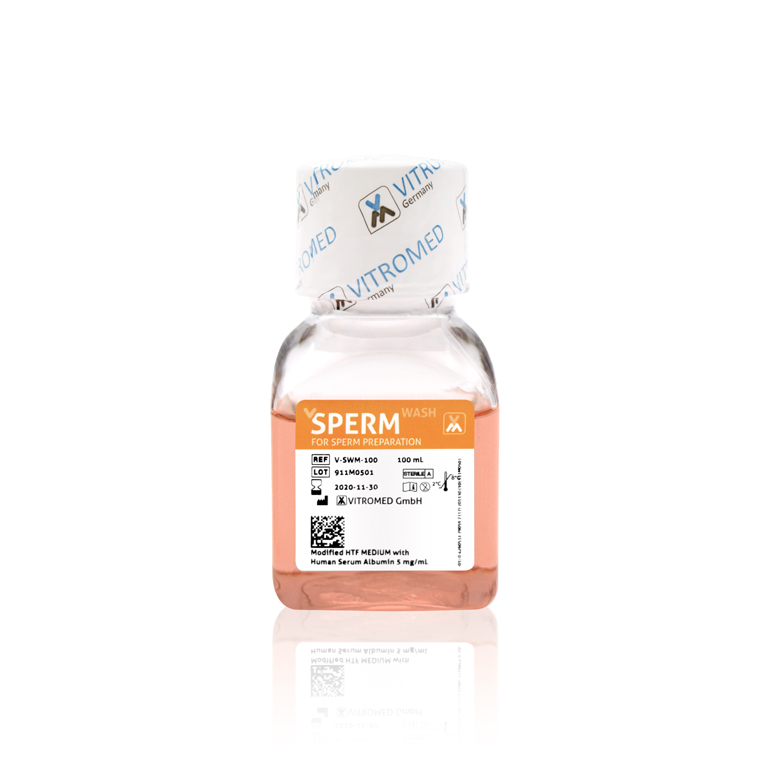
For Sperm Donation (Recipient):
-
Clomid or Letrozole: to induce ovulation
-
Trigger shot: for precise timing of insemination or egg retrieval
🏥 Step 2: Choose a Specialty Fertility Pharmacy
Once you have your prescription, you’ll need to use a fertility-focused pharmacy. These pharmacies are trained in handling time-sensitive medications that require cold storage or precise packaging.
Popular fertility pharmacies in the USA include:
-
Mandell’s Pharmacy
-
Freedom Fertility Pharmacy
-
Integrity Rx
-
Alto Pharmacy
-
Avella Specialty Pharmacy
Your fertility clinic may recommend a partner pharmacy, or you can choose one that works with your insurance and location.
💸 Step 3: Understand the Costs and Insurance Coverage
The cost of fertility medications in the USA can range from $2,000 to $6,000 or more per cycle, depending on your protocol and dosage.
Here’s what to keep in mind:
-
Some private insurance plans may cover medications if you have fertility benefits.
-
Employer-based fertility benefits (via providers like Progyny or Carrot) may include partial or full coverage.
-
Discount programs or pharmacy coupons can lower costs for some brand-name medications.
-
Flexible Spending Accounts (FSA) or Health Savings Accounts (HSA) can often be used to pay for fertility meds.
Be sure to check with both your clinic and your pharmacy about options to reduce costs.
📦 Can Fertility Medications Be Delivered?
Yes! Most fertility pharmacies in the USA offer overnight delivery with temperature-controlled packaging. You will need to:
-
Be available to sign for the package
-
Have access to a refrigerator for storage
-
Follow detailed instructions for mixing and injecting (often provided by the clinic or pharmacy)
⚠️ Safety Tips When Using Fertility Medications
-
Never buy medications from unverified online sources. These can be counterfeit or unsafe.
-
Always check expiration dates and store medications as directed.
-
Train with a nurse or pharmacist if you’re unsure how to administer injections.
-
Keep a calendar or app to track doses and timings — precision is key in fertility protocols.
✅ Final Thoughts
Accessing fertility medications in the USA is a highly regulated but straightforward process when working with licensed professionals. The key is starting with a trusted fertility clinic, obtaining a personalized treatment plan, and working with a reliable fertility pharmacy.
With expert medical support and proper guidance, you can take confident steps toward growing your family — equipped with the medications that make modern fertility treatment so effective.
For any of your fertility problems, please do not hesitate to contact us. At Fertility Solutions we pride ourselves with the excellent tailored personal care we provide to our patients for their specific needs. A team member will contact you as soon as we get your message, and construct a personal treatment plan for your fertility problems in the country of Cyprus. You can also contact our clinics directly through the links below.
Cyprus Crown IVF Contact: https://en.cypruscrownivf.com/contact
Cyprus American IVF Contact: https://www.cyprusamericanivf.com/contact-us/
Dr. Halil Ibrahim Tekin (Dr. HIT) Youtube: https://www.youtube.com/@dr.halilibrahimtekin1715
Cyprus American IVF Youtube: https://www.youtube.com/@AmerikanTupBebekMerkezi