One of the very first questions many fertility patients ask is: “How much does IVF cost?” While completely understandable, this question is often premature. IVF is not a one-size-fits-all treatment — it is a highly individualized medical process that depends entirely on your reproductive health profile.
Before any reputable clinic can provide accurate pricing, several essential diagnostic tests must be completed. These evaluations allow fertility specialists to design a customized treatment strategy, anticipate challenges, and optimize your chances of success.
Simply put — without proper testing, any price you receive is only a rough estimate.
Why Testing Comes Before Pricing
Every fertility journey is biologically unique. Two patients of the same age can have dramatically different ovarian reserves, hormone levels, or uterine conditions.
Providing a price without reviewing medical data can lead to:
-
Unexpected medication costs
-
Cycle cancellations
-
Additional procedures
-
Emotional stress
-
Financial surprises
Leading fertility clinics prioritize medical safety over quick quotations because responsible treatment planning requires evidence, not assumptions.
Think of it like building a home — no architect can give you a precise cost before evaluating the land.
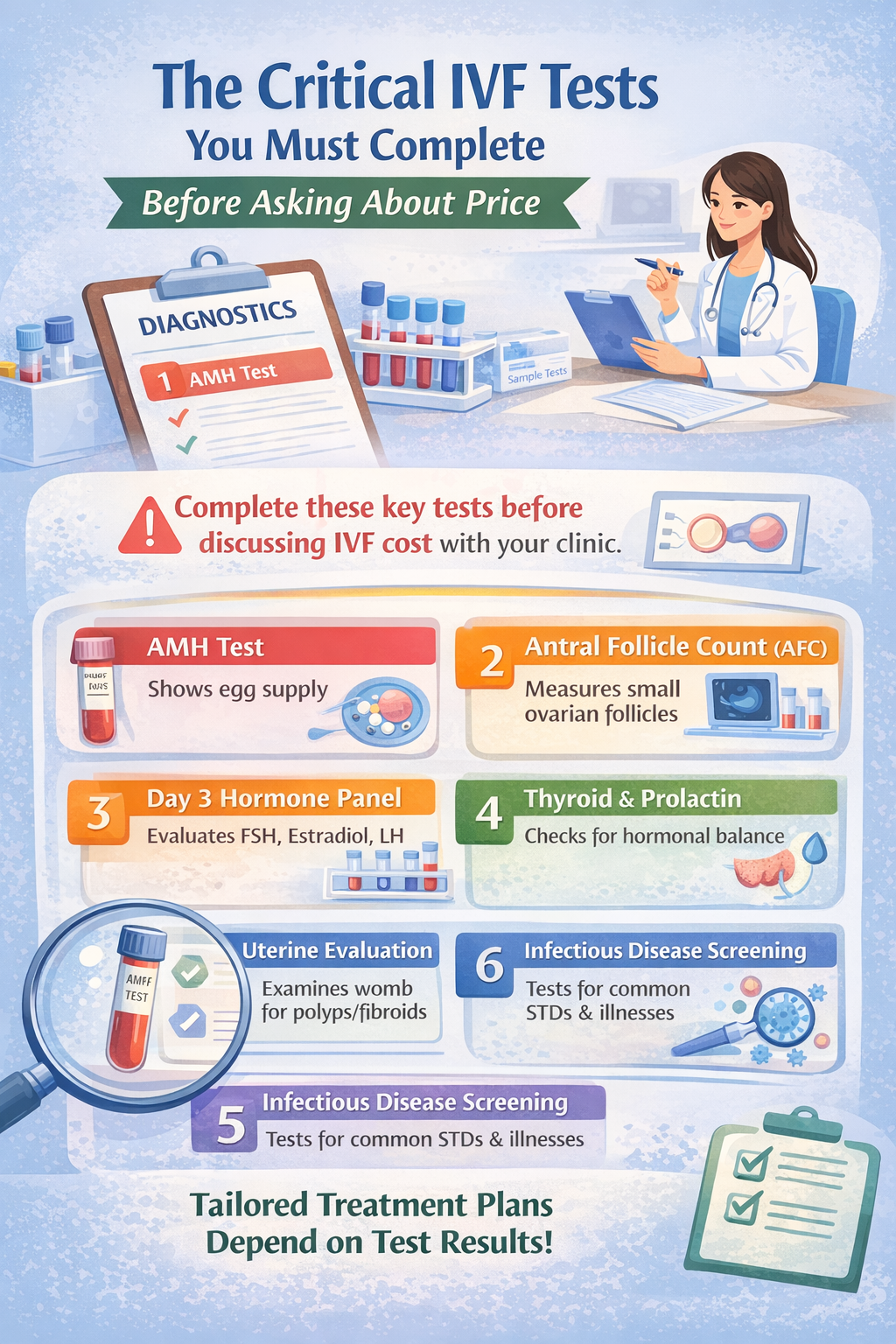
The Most Important IVF Tests When Using Your Own Eggs
1. AMH (Anti-Müllerian Hormone) — The Foundation Test
The AMH test is widely considered the cornerstone of fertility evaluation.
It measures ovarian reserve — essentially estimating how many eggs remain in the ovaries.
Higher AMH does not guarantee pregnancy, but it provides critical insight into how the ovaries are likely to respond to stimulation medications.
Clinics rely heavily on this number to determine:
-
Medication dosage
-
Stimulation protocol
-
Expected egg yield
-
Whether multiple cycles may be recommended
-
Timeline urgency
Most importantly, AMH is what allows physicians to build a truly personalized IVF plan.
Without it, pricing is speculative at best.
2. Antral Follicle Count (AFC)
Performed via transvaginal ultrasound, AFC counts the small follicles visible at the start of the menstrual cycle.
When interpreted alongside AMH, it gives one of the clearest pictures of reproductive potential.
For example:
-
Strong AMH + high AFC → often predicts a better ovarian response
-
Low AMH + low AFC → may require adjusted protocols
This combination is essential for forecasting treatment complexity — and therefore cost.
3. Day 3 Hormone Panel
Typically performed on the third day of menstruation, this blood test evaluates hormones such as:
-
FSH (Follicle-Stimulating Hormone)
-
Estradiol
-
LH
Elevated FSH levels may signal that the ovaries need stronger stimulation, which can influence medication planning.
Again — treatment intensity directly affects overall pricing.
4. Thyroid and Prolactin Testing
Hormonal balance is critical for implantation and early pregnancy.
Even mild thyroid dysfunction can interfere with fertility outcomes, while elevated prolactin levels may disrupt ovulation.
The reassuring part?
These conditions are often easily treatable once identified.
Skipping these tests risks preventable cycle failure.
5. Uterine Evaluation
Before embryo transfer is ever considered, physicians must confirm that the uterus can support implantation.
This may involve:
-
Pelvic ultrasound
-
Saline sonogram
-
Hysteroscopy (if needed)
Detecting polyps, fibroids, or structural irregularities early prevents heartbreaking setbacks later.
6. Infectious Disease Screening
Standard in global fertility care, these tests protect both patients and laboratory environments.
They also ensure embryos are handled according to strict medical safety protocols.
Why Patients Should Resist Shopping for IVF Based on Price Alone
Choosing a fertility clinic purely because it offers the lowest advertised price can be misleading.
Lower initial quotes often exclude:
-
Medication
-
Genetic testing
-
Advanced lab techniques
-
Embryo freezing
-
Additional monitoring
A clinic that insists on reviewing your AMH and diagnostic profile before discussing cost is usually demonstrating medical responsibility — not avoidance.
Transparent pricing begins with accurate diagnosis.
Personalized Medicine Is the Future of IVF
Modern fertility care has shifted away from standardized protocols toward individualized treatment strategies.
Your AMH result acts as a roadmap, guiding physicians toward the safest and most effective approach for your body.
Some patients may benefit from mild stimulation, while others require more advanced protocols. Neither is “better” — only more appropriate for a specific biological situation.
When clinics tailor treatment from the start, patients often experience:
✅ Fewer surprises
✅ Better cycle efficiency
✅ Reduced emotional strain
✅ Greater confidence in their care
Final Thoughts
It is natural to want clarity about financial commitment when considering IVF. However, the smartest first step is not asking, “What is the price?” — it is asking, “What tests do I need?”
Once your AMH and supporting diagnostics are complete, your fertility team can craft a treatment plan designed specifically for you — medically, emotionally, and financially.
Because in reproductive medicine, precision is not a luxury.
It is the foundation of success.
Get in Touch with Our Clinics:
Cyprus Crown IVF Contact: https://en.cypruscrownivf.com/contact
Cyprus American IVF Contact: https://www.cyprusamericanivf.com/contact-us/
Dr. Halil Ibrahim Tekin (Dr. HIT) Youtube: https://www.youtube.com/@dr.halilibrahimtekin1715
Cyprus American IVF Youtube: https://www.youtube.com/@AmerikanTupBebekMerkezi
Clavis Fertility Centre: https://www.clavisfertilitycenter.com