Nourishing the Path to Parenthood: Pre-IVF Nutrition and Folic Acid
The journey to parenthood can be a complex one, and for those embarking on the path of In Vitro Fertilization (IVF), nutrition plays a crucial role. Pre-IVF nutrition not only helps optimize the chances of a successful pregnancy but also sets the foundation for a healthy start for both the mother and the baby. In this blog post, we will explore the importance of nutrition, the role of folic acid, and the avoidance of harmful substances as essential components of pre-IVF preparation.
The Significance of Pre-IVF Nutrition
Before diving into the specifics of pre-IVF nutrition, it’s essential to understand why it matters:
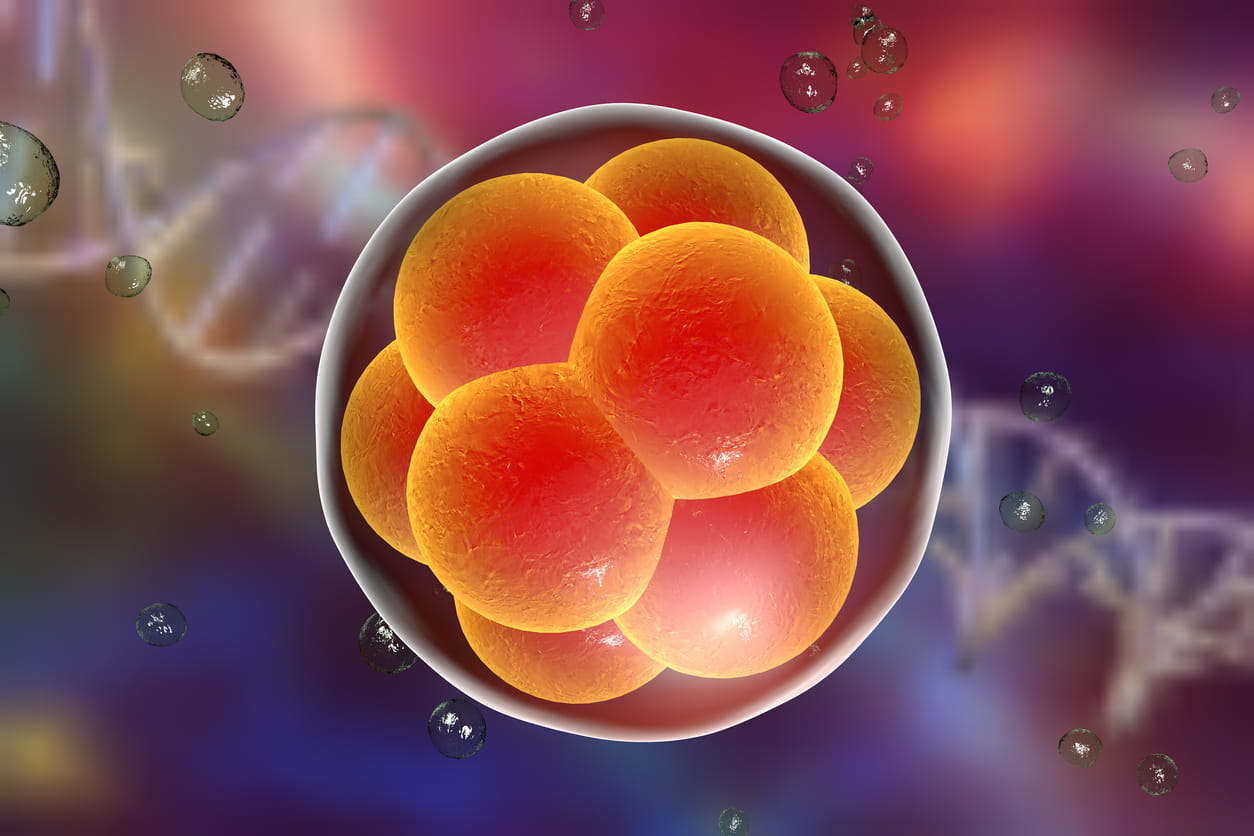
- Optimizing Egg and Sperm Health: Nutrient-rich foods provide the essential vitamins and minerals needed for healthy egg and sperm development, increasing the likelihood of successful fertilization.
- Balancing Hormones: A well-rounded diet helps regulate hormones, crucial for menstrual cycle regularity and egg maturation, both of which are essential for IVF success.
- Reducing Inflammation: Chronic inflammation can negatively impact fertility. A nutritious diet can help reduce inflammation, creating a more favorable environment for conception.
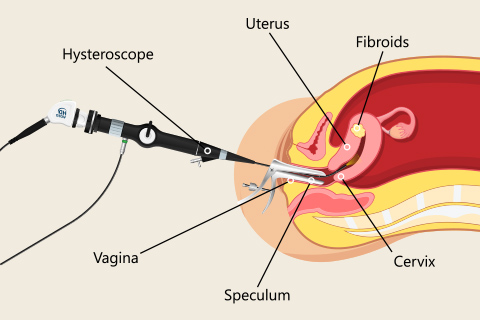
- Supporting the Uterine Lining: Adequate nutrition ensures a healthy uterine lining, which is essential for embryo implantation during IVF.
Folic Acid: A Key Player
Folic acid, a synthetic form of folate (vitamin B9), is a standout nutrient in the realm of pre-IVF nutrition. Here’s why it’s so important:
1. Neural Tube Development: Folic acid is crucial for the early development of the baby’s neural tube, which eventually becomes the brain and spinal cord. Adequate folate intake reduces the risk of neural tube defects, such as spina bifida.
2. DNA Synthesis: Folic acid plays a pivotal role in DNA synthesis and repair, critical processes during the rapid cell division that occurs during pregnancy.
3. Blood Cell Formation: Folate is involved in red blood cell formation, which helps prevent anemia during pregnancy.
4. Risk Reduction: Ensuring sufficient folic acid intake before conception reduces the risk of preterm birth, low birth weight, and other complications.
Incorporating Folic Acid into Pre-IVF Nutrition
To harness the benefits of folic acid, consider the following dietary sources and supplementation:
- Leafy Greens: Foods like spinach, kale, and collard greens are rich in folate.
- Fortified Foods: Many breakfast cereals, bread, and pasta are fortified with folic acid.
- Legumes: Beans, lentils, and peas are excellent natural sources of folate.
- Citrus Fruits: Oranges, grapefruits, and lemons are not only refreshing but also high in folate.
- Supplements: In some cases, healthcare providers may recommend folic acid supplements, especially if dietary intake is insufficient.
Avoidance of Harmful Substances
While adopting a nutritious diet is vital, it’s equally crucial to steer clear of substances that can harm fertility and pregnancy outcomes:
- Alcohol: Excessive alcohol consumption can disrupt hormonal balance and reduce fertility. It’s best to limit or eliminate alcohol intake while trying to conceive.
- Caffeine: High caffeine intake has been linked to fertility problems and a higher risk of miscarriage. Reducing caffeine consumption or switching to decaffeinated options can be beneficial.
- Tobacco and Smoking: Smoking has a detrimental impact on fertility and increases the risk of miscarriage and birth defects. Quitting smoking is essential for pre-IVF preparation.
- Illicit Drugs: The use of recreational drugs can severely impair fertility and pose significant risks during pregnancy. Seek professional help to overcome substance abuse.
Pre-IVF nutrition is not just about increasing the odds of a successful IVF cycle but also about nurturing a healthy start for your future family. Prioritizing nutrient-rich foods, with a special focus on folic acid, provides a strong foundation for the journey ahead. Equally important is the avoidance of harmful substances that can hinder fertility and pregnancy outcomes.
As you embark on your path to parenthood through IVF, remember that nourishing your body with the right foods and making healthy lifestyle choices can contribute to the success of your journey. Consult with a healthcare provider or nutritionist to create a personalized pre-IVF nutrition plan tailored to your specific needs and goals.