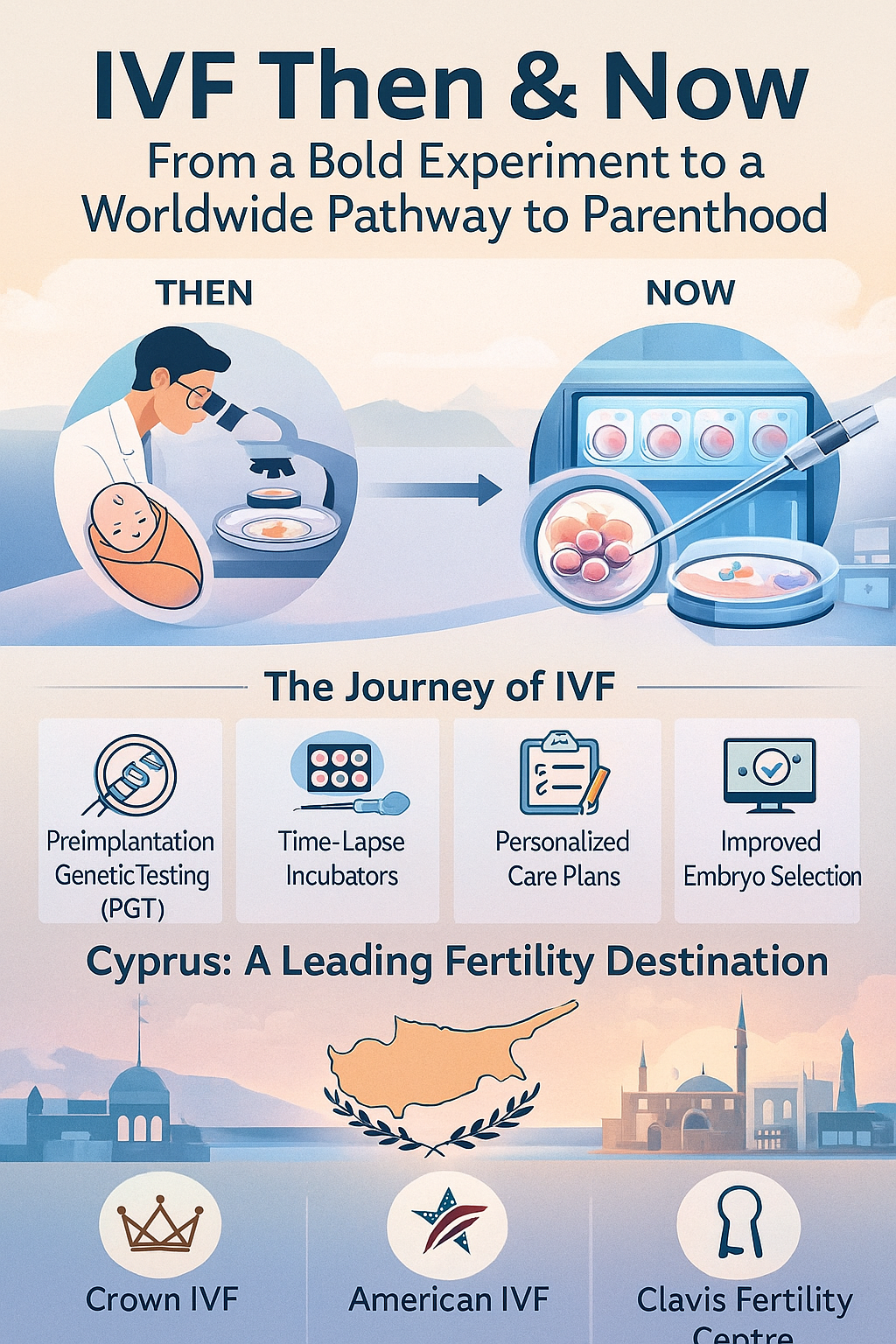
When the world welcomed Louise Brown in 1978—the first baby conceived through in-vitro fertilization (IVF)—reproductive medicine crossed from hopeful theory into life-changing reality. In the decades since, IVF has grown from a pioneering experiment into a trusted global treatment helping millions of families. Today, advances in genetics, lab science, and cryobiology continue to push success rates higher while making the process safer and more individualized.
How IVF Began
The principle of IVF is beautifully simple: retrieve mature eggs from the ovaries, fertilize them with sperm in a carefully controlled laboratory, and transfer one healthy embryo back to the uterus. Early researchers spent years learning how to replicate the body’s natural conditions outside of it—hence the Latin term in vitro (“in glass”).
After Louise Brown’s birth, IVF rapidly spread worldwide. By 1981, clinics in the United States had joined the effort, and through the 1980s and 1990s improvements in ovarian stimulation, embryo transfer, and culture media steadily boosted results.
A major milestone arrived in 1992 with intracytoplasmic sperm injection (ICSI)—the technique of injecting a single sperm directly into an egg. ICSI revolutionized treatment for severe male-factor infertility and expanded IVF’s reach to countless couples. Later innovations such as vitrification (rapid freezing of eggs and embryos) dramatically improved survival after thawing and opened doors for elective egg freezing and long-term embryo storage.
Inside the Modern IVF Laboratory
Today’s embryology labs look nothing like their early counterparts. Some of the most important advances include:
-
Time-lapse embryo imaging: Specialized incubators record embryo growth continuously without disturbing the stable environment, allowing embryologists to choose the healthiest embryos.
-
Preimplantation genetic testing (PGT): Screening embryos for chromosomal or genetic conditions can help reduce miscarriage risk and improve implantation in selected cases.
-
Personalized ovarian stimulation: Tailoring medication protocols to each woman’s hormone profile and history improves egg quality and reduces discomfort.
-
Advanced lab quality systems: Precision air filtration, pH control, and temperature regulation create ideal conditions for embryo development.
The result is a process that is both scientifically precise and more comfortable for patients than ever before.
Cyprus: A Mediterranean Fertility Hub
Over the past decade, Cyprus has emerged as a leading destination for fertility care, attracting patients from Europe, the UK, the Middle East, and North America. The island offers a welcoming atmosphere, English-speaking professionals, and highly regulated clinics equipped with cutting-edge technology—all in a relaxed Mediterranean setting.
Two clinics stand out for their strong reputations and personalized approach:
-
Cyprus Crown IVF – Led by Dr. Halil İbrahim Tekin, one of the island’s most experienced specialists, Cyprus Crown IVF is known for its high success rates and decades of dedication to fertility medicine. The clinic emphasizes patient comfort, transparency, and excellence in embryology laboratory standards.
-
Clavis Fertility Centre – Under Dr. Selen Eçemiş, this modern, purpose-built centre offers spacious facilities, attentive patient care, and a youthful energy that combines precision science with a warm, supportive environment.
Both centers serve local and international patients, providing complete IVF and ICSI programs, egg and sperm donation options, fertility preservation, and comprehensive support for travel and logistics.
The Future of IVF
Looking ahead, several exciting directions are shaping the next era of reproductive medicine:
-
AI-enhanced embryo selection: Artificial intelligence tools are being trained to assist embryologists in identifying embryos with the highest implantation potential—always under human supervision.
-
Evidence-based “add-ons”: The field is becoming more selective about which optional treatments truly improve outcomes, helping patients invest in interventions that matter most.
-
Gentler stimulation protocols: Clinics increasingly use mild stimulation regimens to balance egg yield with patient comfort.
-
Expanded fertility preservation: Egg freezing is now common for women who want flexibility in family planning.
-
Holistic, patient-centered care: Emotional support, nutrition counseling, and mental-health guidance are becoming integral to fertility treatment plans.
Choosing the Right Clinic
Whether you’re starting IVF for the first time or exploring options abroad, look for clinics that prioritize:
-
Clear diagnostic evaluation and individualized treatment planning
-
Transparent success statistics by age and diagnosis
-
Highly trained embryologists and modern lab conditions
-
Evidence-based medical practices rather than routine “extras”
-
Compassionate patient coordination and multilingual support
These factors make a measurable difference in comfort and confidence throughout your journey.
A Hopeful Legacy
From the first IVF birth to today’s advanced laboratories in Cyprus and beyond, the progress in assisted reproduction represents one of modern medicine’s most uplifting success stories. For many hopeful parents, clinics like Cyprus Crown IVF and Clavis Fertility Centre symbolize that powerful blend of science, empathy, and dedication that turns dreams into reality.
Each embryo cultivated in these labs carries not only biological potential but the story of human perseverance—proof that, with the right care, the path to parenthood can begin in the most extraordinary way.
For any of your fertility problems, please do not hesitate to contact us. At Fertility Solutions we pride ourselves with the excellent tailored personal care we provide to our patients for their specific needs. A team member will contact you as soon as we get your message, and construct a personal treatment plan for your fertility problems in the country of Cyprus. You can also contact our clinics directly through the links below.
Get in Touch with Our Clinics:
Cyprus Crown IVF Contact: https://en.cypruscrownivf.com/contact
Cyprus American IVF Contact: https://www.cyprusamericanivf.com/contact-us/
Dr. Halil Ibrahim Tekin (Dr. HIT) Youtube: https://www.youtube.com/@dr.halilibrahimtekin1715
Cyprus American IVF Youtube: https://www.youtube.com/@AmerikanTupBebekMerkezi